I mentioned in my previous post, SphincterWeakness, the ALS Association’s PDF guide on Swallowingand Swallowing Disorders. Several readers asked questions concerning
swallowing issues they are experiencing. Until I read the guide, I never
understood how complicated the entire process is and the coordination needed,
both voluntary and involuntary, to make the process successful. Today’s post is
taken from the guide and is a primer on the swallowing process. I hope you find
it as interesting as I did.
U N D E R STA N D I N G SWA L LOW I N G
The Normal Swallowing Process
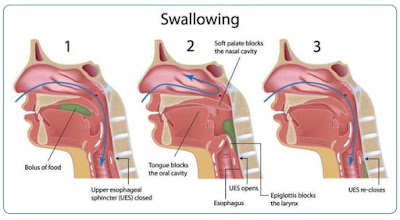
The primary purpose of swallowing is to safely transport food and liquid from the mouth to the stomach. The act of swallowing is a complex process that involves approximately 26 pairs of muscles and five cranial nerves that work together to propel food from your mouth to the stomach.
The swallowing process has been divided into four conceptual
stages, namely the oral preparatory, oral, pharyngeal, and esophageal stages.
Typically, food and liquid pass from our mouth and through our throat in less
than two seconds, however, the sequence of events is very involved. The
following events occur during each stage:
Oral Preparatory Stage: Food is placed into the mouth either with a feeding utensil (fork or spoon), fingers, cup, or straw, and then is chewed and prepared for swallowing. This typically involves a hand-to-mouth transfer motion as food is taken from a plate and placed into the mouth, or when a cup is picked up and placed at the lips for drinking.
Oral Stage: The muscles of the mouth, jaw, and tongue work to prepare the food material for swallowing. This involves chewing and grinding food materials into smaller participles. During chewing and grinding of food materials, your saliva mixes with the ingested material to aid in forming a cohesive “bolus” that can be easily swallowed. Once the bolus is formed, muscles of the tongue work to push the food/liquid from the front to the back of the mouth and towards the throat.
At this time, it is important for the lips to tightly close
or seal off the mouth and for the muscles of the roof of the mouth (soft
palate) to close off the entrance to the nose (nasal cavity). This ensures that
food and liquid are directed into the throat and ensure that it does not escape
out of the mouth or the nasal cavity.
Pharyngeal Stage: Once the ingested materials pass the tonsils, the pharyngeal stage of swallowing begins and the swallowing process becomes involuntary (not under your conscious control). The cylindrical throat muscles squeeze to help push the food from the upper throat, through a ring muscle at the bottom of the throat surrounding the opening of the food pipe (medical term: sphincter), into the food pipe (medical term: esophagus).
During this stage of swallowing, entrance to the airway
(medical term: trachea) is protected by a flap of cartilage called the
epiglottis. This flips over (down) during the swallow to route food/liquid away
from the airway and towards the stomach and has often been referred to as the
“guardian angel” of the airway. Two additional barriers occur during this stage
to protect your airway, consisting of the closure of both the false and true
vocal folds at the entrance to your trachea or airway.
Esophageal Stage:
The ring muscle that divides the throat from the entry to the food pipe
(medical term: Upper Esophageal Sphincter or UES) is usually closed to prevent
1) air from entering the stomach and 2) previously ingested food and liquid
materials from coming back up into the throat (reflux or regurgitation). This
sphincter briefly opens or relaxes during the swallow and at the start of the
esophageal stage to allow both food and liquid to enter the food pipe (Figure 1).
Once food or liquids enter the esophagus, or food pipe, a contraction of the muscle helps to move the food from the top to the bottom of the pipe (21-27
cm in length) and into the stomach.